© All rights reserved galwayclinic.com 2013

Pulmonary vein ablation / Atrial fibrillation
Pulmonary vein ablation procedure:
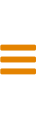
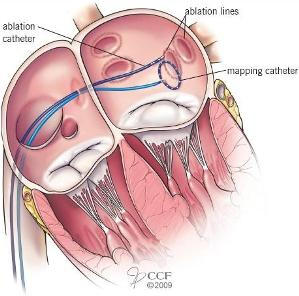
Energy is delivered through the tip of the catheter to tissue that is targeted for ablation. The energy is applied in a circle around the connection of the left upper and lower pulmonary veins to the left atrium. A roof line is created between the right and left upper pulmonary veins to target electrical tissue along the roof of the left atrium. This cautery or ablation prevents electrical impulses from the pulmonary veins or roof entering the atrium and putting the heart out of rhythm.What happens during the ablation procedure?
During pulmonary vein ablation, an electrophysiologist inserts electrical recording catheters into the blood vessels of the leg and guides the catheters into the atrium. Energy is delivered through the tip of the catheter to tissue that is targeted for ablation. The energy is applied around the connections of the pulmonary veins to the left atrium. A roof line is created between the upper veins to isolate the roof of the atrium. Frequently, other areas involved in triggering or maintaining atrial fibrillation are also targeted. The ablation procedure is done using anaesthesia so you will wake up when the procedure is completed. You are monitored by an anaesthesist together with the electrophysiologist and specialist cardiac nurses. An ultrasound catheter is placed through a leg vein into the heart to view the structures of the heart and evaluate the position of the catheters during the procedure. During the procedure the cardiologist is viewing x-ray screens showing the catheter positions and continuous electrical recordings of the heart are being studied. Small circular scars eventually form and prevent the abnormal signals that cause atrial fibrillation from reaching the rest of the atrium. However, the scars created during this procedure may take from 2 to 3 months to form. Once the scars form, they block any impulses firing from within the pulmonary veins, thereby electrically “disconnecting” them or “isolating” them from the heart. This allows the SA node to once again direct the heart rhythm and a normal sinus rhythm is restored. Because it takes several weeks for the lesions to heal and form scars, it is not uncommon to experience atrial fibrillation early during the recovery period. Rarely, atrial fibrillation may be worse for a few weeks after the procedure and may be related to inflammation where the lesions were created. In most patients, these episodes subside within 1 to 3 months. Patients have a CT scan of their chest to study the pulmonary veins the day before the procedure.
Galway Clinic Facebook page
Tel: +353 (0) 91720170 brendan.ocochlain@galwayclinic.com
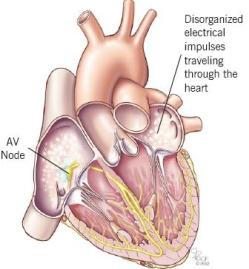
Rapid firing impulses
With atrial fibrillation, many different impulses rapidly fire at once, causing a very fast, chaotic rhythm. The resulting heartbeat is irregular, ranging from 100 to 200 beats per minute. To determine if ablation is an appropriate treatment, a thorough evaluation will be performed, which may include: • A review of your medical history • Complete physical examination • Electrocardiogram (ECG) • Echocardiogram (echo - an ultrasound to evaluate your heart function and heart valves) • Holter monitor test (a 24-hour ECG) After the evaluation, the doctor will talk with you about your treatment options. Monitors used during the procedure PVI - atrial flutter ablation Several monitors will be used during the procedure to check your heart rhythm and your body’s responses to any arrhythmias that occur. • Defibrillator/pacemaker/cardioverter: Attached via wires to one sticky patch placed on the center of your back and one on your chest. This device allows the doctor and nurse to pace your heart rate if it is too slow, or deliver energy to your heart if the rate is too fast. • Electrocardiogram: Attached to several sticky electrode patches placed on your chest. Provides a picture on the monitors of the electrical impulses traveling through the heart. • Blood pressure monitor: Connected to a blood pressure cuff on your arm. Checks your blood pressure throughout the procedure. • Mapping system: State-of-the-art recording technology using catheters inside the heart to help your doctor locate the exact area of your arrhythmia. • Ablation machine: Attached to another sticky patch on your back. • Oximeter monitor: Attached to a small clip placed on your finger. Checks the oxygen level of your blood. • Fluoroscopy: A large X-ray machine will be positioned above you to help the doctors see the leads on an X-ray screen during the procedure. • Intracardiac ultrasound: Performed by a catheter transducer inserted into the heart: Used throughout the procedure to view the structures of the heart and the catheter when it is in contact with the heart lining. A catheter in the left atrium is used to find or map the abnormal impulses coming from the pulmonary veins. This catheter has multiple electrodes that allow a circular ablation to be performed by delivering energy between the electrodes. This creates a circular scar around the openings of the veins preventing electrical impulses from reaching the heart. Each vein in turn is targeted until all the electrical signals in the veins are ablated.What can I expect after the procedure?
Overnight Hospital Stay: You will be admitted to the hospital and stay for 2-3 nights after the procedure for observation. In your hospital room, a telemetry monitor will be used to evaluate your heart rate and rhythm during your recovery. Telemetry consists of a small box connected by wires to your chest with sticky electrode patches. The box displays your heart rhythm on several monitors Activity: Usually you can return to your normal activities within 48 hours after the procedure. For one week after the procedure, you cannot lift anything that weighs more than 10 pounds. You should wait at least three weeks before you resume intense exercise. Medications: You will receive the necessary prescriptions and medication instructions from your doctor. Ask your doctor if you should keep taking the medications you took before you had the procedure. In some cases, your doctor may recommend additional treatments or medicationsSuccess rate for single ablation procedure
The success rate for a single pulmonary vein ablation procedure depends on several factors. The highest cure rate is achieved in patients with paroxysmal atrial fibrillation in whom atrial fibrillation stops on its own within 1 to 3 days. At the Galway Clinic a single pulmonary vein ablation procedure is completely curative in approximately 85 to 90 percent of patients with paroxysmal atrial fibrillation that is not associated with any other heart disease. We are now seeing many patients with Atrial fibrillation that has been present for several years on and off and patients that have had procedures at other hospitals. Our success rate in controlling their Atrial fibrillation which is more advanced is also very high. An ablation procedure is not likely to cure patients who have had continuous Atrial fibrillation for many years without normal heart rhythm being restored. These patients have extensive scarring in the atrium and dilated atria as a result.Long term treatment goal
The long-term goal of the pulmonary vein ablation procedure is to eliminate the need for medications to prevent atrial fibrillation. Most patients can stop taking blood thinners a few months after the procedure, as long as they do not have a high risk of stroke. Even patients who are not completely cured of atrial fibrillation may benefit from the ablation procedure because the procedure helps them have a better response to medications that were previously ineffective.When is pulmonary vein ablation appropriate?
For patients with recurrent symptoms despite treatment with antiarrhythmic medications For patients unable to take or having side effects with medications For young patients with no other medical conditions who would like to avoid long term medications For patients with poorly controlled symptoms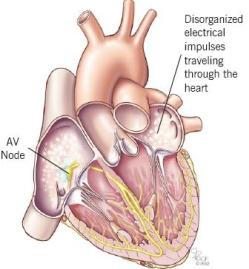

Galway Site Design

Pulmonary vein ablation / Atrial fibrillation
Pulmonary vein ablation procedure:
Energy is delivered through the tip of the catheter to tissue that is targeted for ablation. The energy is applied in a circle around the connection of the left upper and lower pulmonary veins to the left atrium. A roof line is created between the right and left upper pulmonary veins to target electrical tissue along the roof of the left atrium. This cautery or ablation prevents electrical impulses from the pulmonary veins or roof entering the atrium and putting the heart out of rhythm.What happens during the ablation procedure?
During pulmonary vein ablation, an electrophysiologist inserts electrical recording catheters into the blood vessels of the leg and guides the catheters into the atrium. Energy is delivered through the tip of the catheter to tissue that is targeted for ablation. The energy is applied around the connections of the pulmonary veins to the left atrium. A roof line is created between the upper veins to isolate the roof of the atrium. Frequently, other areas involved in triggering or maintaining atrial fibrillation are also targeted. The ablation procedure is done using anaesthesia so you will wake up when the procedure is completed. You are monitored by an anaesthesist together with the electrophysiologist and specialist cardiac nurses. An ultrasound catheter is placed through a leg vein into the heart to view the structures of the heart and evaluate the position of the catheters during the procedure. During the procedure the cardiologist is viewing x-ray screens showing the catheter positions and continuous electrical recordings of the heart are being studied. Small circular scars eventually form and prevent the abnormal signals that cause atrial fibrillation from reaching the rest of the atrium. However, the scars created during this procedure may take from 2 to 3 months to form. Once the scars form, they block any impulses firing from within the pulmonary veins, thereby electrically “disconnecting” them or “isolating” them from the heart. This allows the SA node to once again direct the heart rhythm and a normal sinus rhythm is restored. Because it takes several weeks for the lesions to heal and form scars, it is not uncommon to experience atrial fibrillation early during the recovery period. Rarely, atrial fibrillation may be worse for a few weeks after the procedure and may be related to inflammation where the lesions were created. In most patients, these episodes subside within 1 to 3 months. Patients have a CT scan of their chest to study the pulmonary veins the day before the procedure.
Galway Clinic Facebook page


Rapid firing impulses
With atrial fibrillation, many different impulses rapidly fire at once, causing a very fast, chaotic rhythm. The resulting heartbeat is irregular, ranging from 100 to 200 beats per minute. To determine if ablation is an appropriate treatment, a thorough evaluation will be performed, which may include: • A review of your medical history • Complete physical examination • Electrocardiogram (ECG) • Echocardiogram (echo - an ultrasound to evaluate your heart function and heart valves) • Holter monitor test (a 24-hour ECG) After the evaluation, the doctor will talk with you about your treatment options. Monitors used during the procedure PVI - atrial flutter ablation Several monitors will be used during the procedure to check your heart rhythm and your body’s responses to any arrhythmias that occur. • Defibrillator/pacemaker/cardioverter: Attached via wires to one sticky patch placed on the center of your back and one on your chest. This device allows the doctor and nurse to pace your heart rate if it is too slow, or deliver energy to your heart if the rate is too fast. • Electrocardiogram: Attached to several sticky electrode patches placed on your chest. Provides a picture on the monitors of the electrical impulses traveling through the heart. • Blood pressure monitor: Connected to a blood pressure cuff on your arm. Checks your blood pressure throughout the procedure. • Mapping system: State-of-the-art recording technology using catheters inside the heart to help your doctor locate the exact area of your arrhythmia. • Ablation machine: Attached to another sticky patch on your back. • Oximeter monitor: Attached to a small clip placed on your finger. Checks the oxygen level of your blood. • Fluoroscopy: A large X-ray machine will be positioned above you to help the doctors see the leads on an X-ray screen during the procedure. • Intracardiac ultrasound: Performed by a catheter transducer inserted into the heart: Used throughout the procedure to view the structures of the heart and the catheter when it is in contact with the heart lining. A catheter in the left atrium is used to find or map the abnormal impulses coming from the pulmonary veins. This catheter has multiple electrodes that allow a circular ablation to be performed by delivering energy between the electrodes. This creates a circular scar around the openings of the veins preventing electrical impulses from reaching the heart. Each vein in turn is targeted until all the electrical signals in the veins are ablated.What can I expect after the procedure?
Overnight Hospital Stay: You will be admitted to the hospital and stay for 2-3 nights after the procedure for observation. In your hospital room, a telemetry monitor will be used to evaluate your heart rate and rhythm during your recovery. Telemetry consists of a small box connected by wires to your chest with sticky electrode patches. The box displays your heart rhythm on several monitors Activity: Usually you can return to your normal activities within 48 hours after the procedure. For one week after the procedure, you cannot lift anything that weighs more than 10 pounds. You should wait at least three weeks before you resume intense exercise. Medications: You will receive the necessary prescriptions and medication instructions from your doctor. Ask your doctor if you should keep taking the medications you took before you had the procedure. In some cases, your doctor may recommend additional treatments or medicationsSuccess rate for single ablation procedure
The success rate for a single pulmonary vein ablation procedure depends on several factors. The highest cure rate is achieved in patients with paroxysmal atrial fibrillation in whom atrial fibrillation stops on its own within 1 to 3 days. At the Galway Clinic a single pulmonary vein ablation procedure is completely curative in approximately 85 to 90 percent of patients with paroxysmal atrial fibrillation that is not associated with any other heart disease. We are now seeing many patients with Atrial fibrillation that has been present for several years on and off and patients that have had procedures at other hospitals. Our success rate in controlling their Atrial fibrillation which is more advanced is also very high. An ablation procedure is not likely to cure patients who have had continuous Atrial fibrillation for many years without normal heart rhythm being restored. These patients have extensive scarring in the atrium and dilated atria as a result.Long term treatment goal
The long-term goal of the pulmonary vein ablation procedure is to eliminate the need for medications to prevent atrial fibrillation. Most patients can stop taking blood thinners a few months after the procedure, as long as they do not have a high risk of stroke. Even patients who are not completely cured of atrial fibrillation may benefit from the ablation procedure because the procedure helps them have a better response to medications that were previously ineffective.When is pulmonary vein ablation appropriate?
For patients with recurrent symptoms despite treatment with antiarrhythmic medications For patients unable to take or having side effects with medications For young patients with no other medical conditions who would like to avoid long term medications For patients with poorly controlled symptoms